For a long time, deafness has often been misunderstood, fueling segregation against people who are deaf or hard of hearing. In some communities, it is still seen as a curse or divine punishment; in others, it’s treated as an inevitable part of ageing.
However, modern science offers a significantly different perspective. While the majority of hearing loss worldwide is acquired later in life, often due to infections, noise exposure, or chronic illnesses, a significant number of cases are hereditary, with roots in our genes long before birth.
In Nigeria and across much of Africa, the conversation about hereditary deafness remains limited. Prenatal screenings are rare, data is sparse, and stigma is widespread.
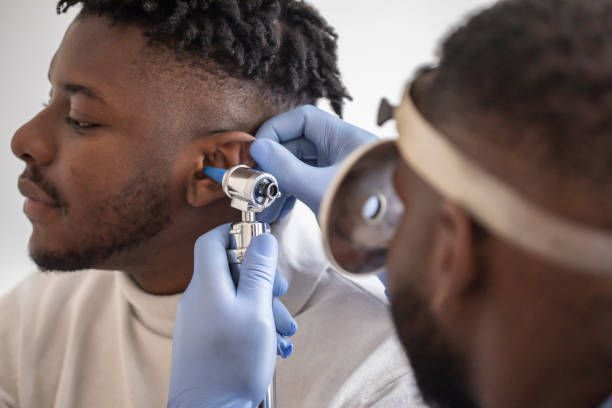
To unpack what we actually know about hereditary deafness and separate fact from myth, we spoke with two medical professionals: Dr Badru Muhydeen Damilola, a medical doctor passionate about genetic diseases and improving African participation in genetic research, and Dr Abel Samuel Paul, an ENT specialist.
Their insights reveal that hereditary deafness is far more nuanced than most people realise, and that tackling bias is just as important as advancing science.
What causes deafness, and how much of it is hereditary?
Both doctors agree that the term “deafness” is usually reserved for the most severe form of hearing loss, specifically profound hearing impairment, which exceeds 81 decibels as prescribed by World Health Organisation (WHO) standards.
However, hearing loss exists on a spectrum, ranging from mild impairments, such as earwax impaction, to profound congenital conditions, like Mondini ear deformity.
Dr Badru explains that in Africa, the majority of hearing loss is acquired. Leading causes include recurrent ear infections (otitis media), birth and neonatal complications (like severe jaundice or birth asphyxia), ear wax impaction, prolonged noise exposure, harmful drugs and chemicals (including tobacco), age-related decline, and chronic diseases like diabetes. However, hereditary factors become more prominent in cases of profound deafness.
Dr Paul adds that while genetics can predispose someone to hearing loss, environmental factors often determine its severity. “Not everyone who grows old will have deafness if we exclude environmental factors,” he says. In other words, genes may create vulnerability, but circumstances often trigger its manifestation.
What does it mean for deafness to be hereditary?
When we say deafness is hereditary, it means the condition can be passed from parent to child through genes.
But as Dr Badru notes,
it’s misleading to think all or most deafness is genetic. While congenital [present at birth] hearing loss is mostly hereditary in Western countries, accounting for more than 50–60% of cases, this is only one part of the picture. Infections, maternal illnesses, or exposure to toxic drugs during pregnancy also cause hearing impairment from birth.
Dr Paul points to genetic conditions like Trisomy 21 (Down syndrome), where chromosomal defects can impact hearing. In Nigeria, however, there’s almost no large-scale data to measure how many cases are truly hereditary.
If parents are deaf, will their children also be deaf?
This is one of the most common fears in families with hearing loss. Dr Badru explains that the genetics of hereditary deafness are far more complex than many people think.
“Western research suggests that deaf-deaf unions of any cause have about 9% deaf offspring, while deaf-hearing marriages yield 13.5% deaf children. In congenital deaf marriages, the likelihood rises to 25%. Yet paradoxically, up to 95% of children with congenital hearing loss are born to hearing parents,” Dr Badru explains.
These patterns reveal the hidden role of genetic inheritance. Aside from the well-known autosomal recessive, autosomal dominant, and X-linked patterns, there is also digenic inheritance, where mutations in two different genes combine to cause hearing loss.
Dr Paul stresses that while genetic counselling and screening exist abroad, such services are almost nonexistent in Nigeria. Prenatal genetic diagnosis isn’t routine here, even for sickle cell disease, a condition with far more public awareness.
How is hereditary deafness managed differently from acquired hearing loss?
Both doctors emphasise that the first step with an infant or young child suspected of having a hearing impairment is to establish whether it’s hereditary.
Dr. Badru describes a comprehensive approach, which includes detailed family histories covering at least three generations, physical exams for ear abnormalities such as preauricular pits or tags, and pregnancy histories to identify maternal illnesses or exposures.
This workup helps classify the primary cause and guides treatment. In acquired cases, treatment often focuses on eliminating the cause (like treating infections or removing earwax). In hereditary cases, early diagnosis is key to management, since the underlying gene can’t yet be “treated away” in Nigeria.
Early intervention, such as the use of hearing aids or cochlear implants, can still significantly improve outcomes.
Are there promising treatments for hereditary deafness?
Yes. Dr Badru highlights developments such as gene-editing technologies for single-gene disorders and Auditory Brainstem Implants, which bypass the ears entirely to send sound signals directly to the brain.
Dr Paul mentions gene therapy trials, such as the OTOF gene therapy for OTOF-related deafness, which have shown significant improvements in hearing.
While these treatments aren’t widely available in Nigeria, they show that the future of managing hereditary deafness may differ radically from today.
Tackling bias and stigma against deaf people
Understanding the science is only part of the story. Deaf people in Nigeria still face biases that limit their opportunities.
From workplaces that assume they’re unfit for specific roles to schools without sign language interpreters, the stigma often isolates them further.
Healthcare systems can make things worse. Licensing offices rarely provide sign language interpreters, and even hospitals may lack staff trained to communicate with deaf patients. These barriers fuel myths and discrimination.
What needs to change?
Clear, unified policy: Agencies like the Federal Road Safety Corps (FRSC) should publicly clarify that deaf people can apply for licences and access services without discrimination.
Training for officials: Basic sign language or written communication skills should be taught to staff at licensing offices, hospitals, and traffic stops to ensure inclusion.
Improved road and public infrastructure: More visible signs, alerts, and accessible information can help deaf people navigate public spaces safely and independently.
Public awareness campaigns: Campaigns should debunk myths about deaf drivers, deaf workers, and deaf students, demonstrating that hearing impairment doesn’t equal incapacity.
Deafness isn’t a consequence of a curse nor is it a single condition; it lies on a spectrum, with causes ranging from infections to inherited genetic conditions.
Both Dr Badru and Dr Paul agree that while most hearing loss in Nigeria is acquired and preventable, hereditary deafness deserves more attention. Without screening, research, and public awareness, families remain in the dark and deaf people continue to face stigma.