Nairobi — African countries have renewed calls for equitable, affordable, and timely access to long-acting HIV prevention and treatment innovations, warning that scientific breakthroughs alone will not end the epidemic without deliberate action to close access and affordability gaps.
The call was made during a high-level UNAIDS meeting in Brazil, where Kenya’s National AIDS and STI Control Programme (NASCOP) Head, Dr Andrew Mulwa, delivered the Africa Regional Statement under Agenda Item 10 on behalf of African Member States.
Addressing delegates, the Ministry of Health disclosed that Dr Mulwa stressed the transformative potential of long-acting antiretroviral medicines (ARVs) in addressing persistent challenges in HIV prevention and treatment, particularly among populations that struggle with daily oral regimens due to social, economic, or structural barriers.
Follow us on WhatsApp | LinkedIn for the latest headlines
The official lauded the AIDS agency and orgnizers of the meeting which he said could not have a come at a better time.
“He commended UNAIDS, the meeting organisers, and technical experts for advancing discussions on practical solutions at a time of increasing pressure on global health systems,” MoH said adding that long-acting technologies could significantly improve adherence, retention in care, and overall health outcomes across the continent.
While acknowledging Africa’s progress in reducing AIDS-related deaths and new HIV infections through expanded access to antiretroviral therapy, Dr Mulwa noted that significant gaps remain, particularly among vulnerable populations.
Pregnant and breastfeeding women living with HIV continue to face treatment interruptions and adherence challenges, contributing to ongoing mother-to-child transmission.
He warned that global efforts are not on track to end AIDS among children by 2030.
Current data shows adult viral suppression at approximately 73 per cent, compared to just 48 per cent among children living with HIV.
Adolescents and young people remain disproportionately affected, with adolescent girls aged 15-19 in sub-Saharan Africa nearly six times more likely to acquire HIV than boys of the same age.
Beyond Africa, Dr Mulwa noted that in regions such as Asia and the Pacific, key populations and their partners account for the majority of new HIV infections among young people, highlighting the global nature of the challenge.
Dr Mulwa also drew attention to the structural and social factors sustaining the epidemic, including poverty, stigma and discrimination, gender-based violence, criminalisation of key populations, and restrictive age-of-consent laws.
These barriers, he said, continue to limit access to prevention, testing, treatment, and care–especially for adolescents.
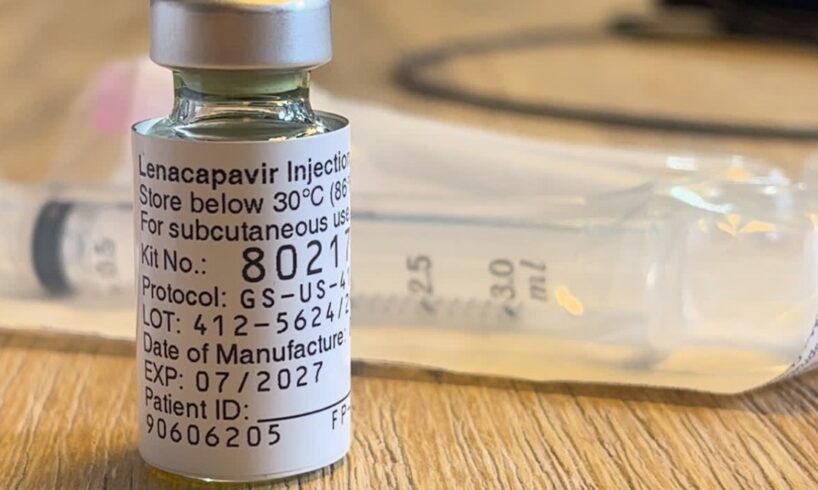
African Member States welcomed long-acting injectable ARVs as a promising innovation to improve adherence and continuity of care.
Sign up for free AllAfrica Newsletters
Get the latest in African news delivered straight to your inbox
Success!
Almost finished…
We need to confirm your email address.
To complete the process, please follow the instructions in the email we just sent you.
Error!
There was a problem processing your submission. Please try again later.
However, Dr Mulwa stressed that their impact will depend on affordability, regulatory readiness, and timely availability across low- and middle-income countries.
He further emphasised that long-acting HIV technologies should complement, not replace, a comprehensive and person-centred response that integrates biomedical interventions with behavioural approaches, condom use, community-led services, and structural reforms aimed at reducing stigma and dismantling legal barriers.
As Africa continues to shoulder more than half of the world’s new HIV infections, Member States urged global partners, pharmaceutical companies, donors, and multilateral institutions to work closely with governments and regional bodies to ensure universal and affordable access to long-acting HIV prevention and treatment options.